FLOURISH recently sat down with Dr. Ebony Carter, a Barnes Jewish Hospital obstetrician and assistant professor in Washington University’s Division of Maternal Fetal Medicine, to get her perspective on implicit bias in the health care system.
“I’ve been teaching and practicing medicine for over 10 years and have observed that the way medical professionals interact with their patients can have a profound impact on their health outcomes,” said Dr. Carter.
Implicit bias refers to when one has attitudes toward persons or people or associates stereotypes with them without one’s conscious knowledge. People may possess this unconscious bias based on race, gender or socioeconomic status.
“Unfortunately no one is immune to implicit bias – even medical professionals,” said Dr. Carter. “Although we may be 100 percent committed to providing quality care to our patients, we walk into the exam room carrying the weight of all of the biases we’ve accumulated throughout life. It is human nature to rely on assumptions and prior life experiences to make shortcuts in decision making. But these decisions lead to inequities and have implications across sectors, including who gets hired for a job, or who gets a good rate on a mortgage; but, life and death can lay in the balance when these shortcuts are applied to medical decision-making.”
Dr. Carter thinks acknowledging that each of us is personally biased, and that we work in systems, organizations, and institutions that perpetuate bias, is the first step in overcoming it. It is impossible to address a problem that one does not believe exists.
“I encourage the trainees who work with me (medical students, residents, and fellows) to speak with patients conversationally with less clinical jargon and take time to get to know their patient and her family better,” says Carter. “By identifying with patients as people and not jumping to conclusions based on society’s pre-conceived notions, we can better deliver the right kind of care for our patients.”
Dr. Carter believes BJC Healthcare and Washington University are starting to do the hard work that is necessary to achieve equitable care for all its patients. All physicians in the Department of Obstetrics and Gynecology are required to attend Unconscious Bias and Inclusion training to equip them with the tools and knowledge to push past their implicit biases to provide more equitable care. Another example is the Centering Pregnancy program, a group prenatal care program modeled from the Centering® Healthcare Institute in Boston. This program provides an opportunity for pregnant women to support each other during regular group interactions, and for medical professionals to spend more time with their patients to better understand their needs and perspectives.
“Ultimately, this culturally-competent approach can lead to better delivery of care as it breaks down time and space barriers in the patient-provider relationship and has better pregnancy outcomes. It’s a win-win,” said Dr. Carter.
Training more diverse doctors is another bias-reducing strategy. Studies show providers of the same race or similar background as their patients help improve communication and trust.
“As an African-American woman in a field where most people do not look like me, I work hard to pave the way for those who come behind me through mentorship and advocate for patients, especially those who are least likely to have a seat at the table or a voice.”
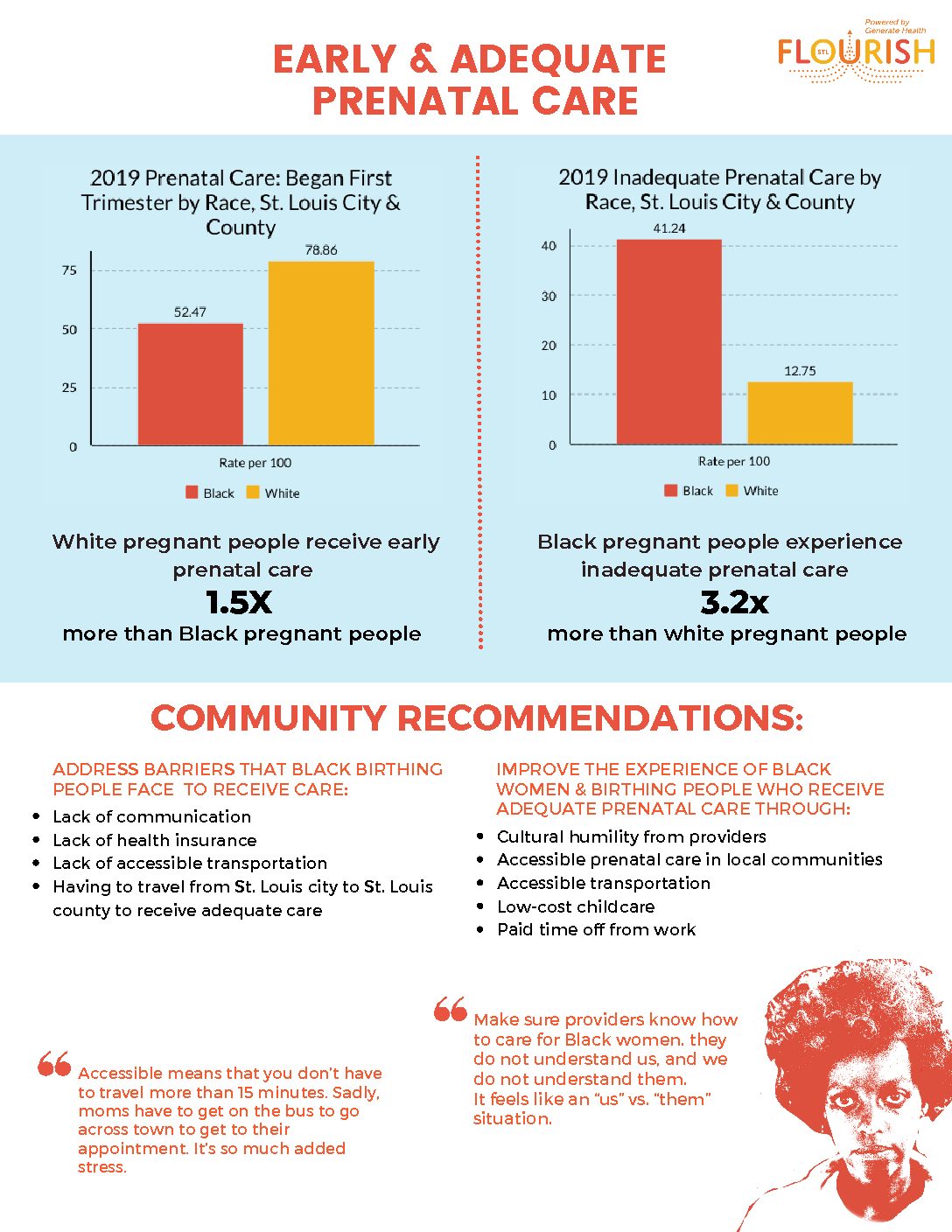
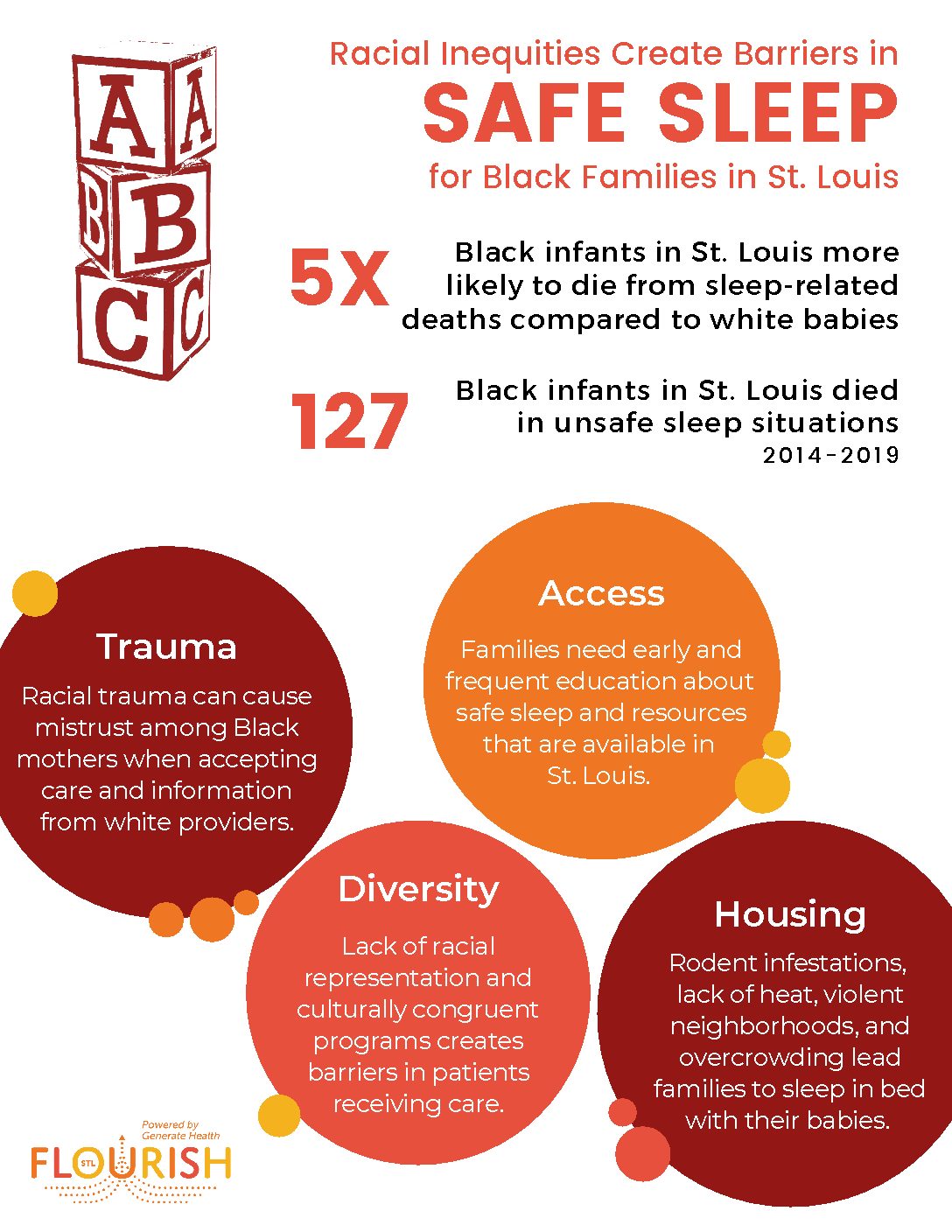
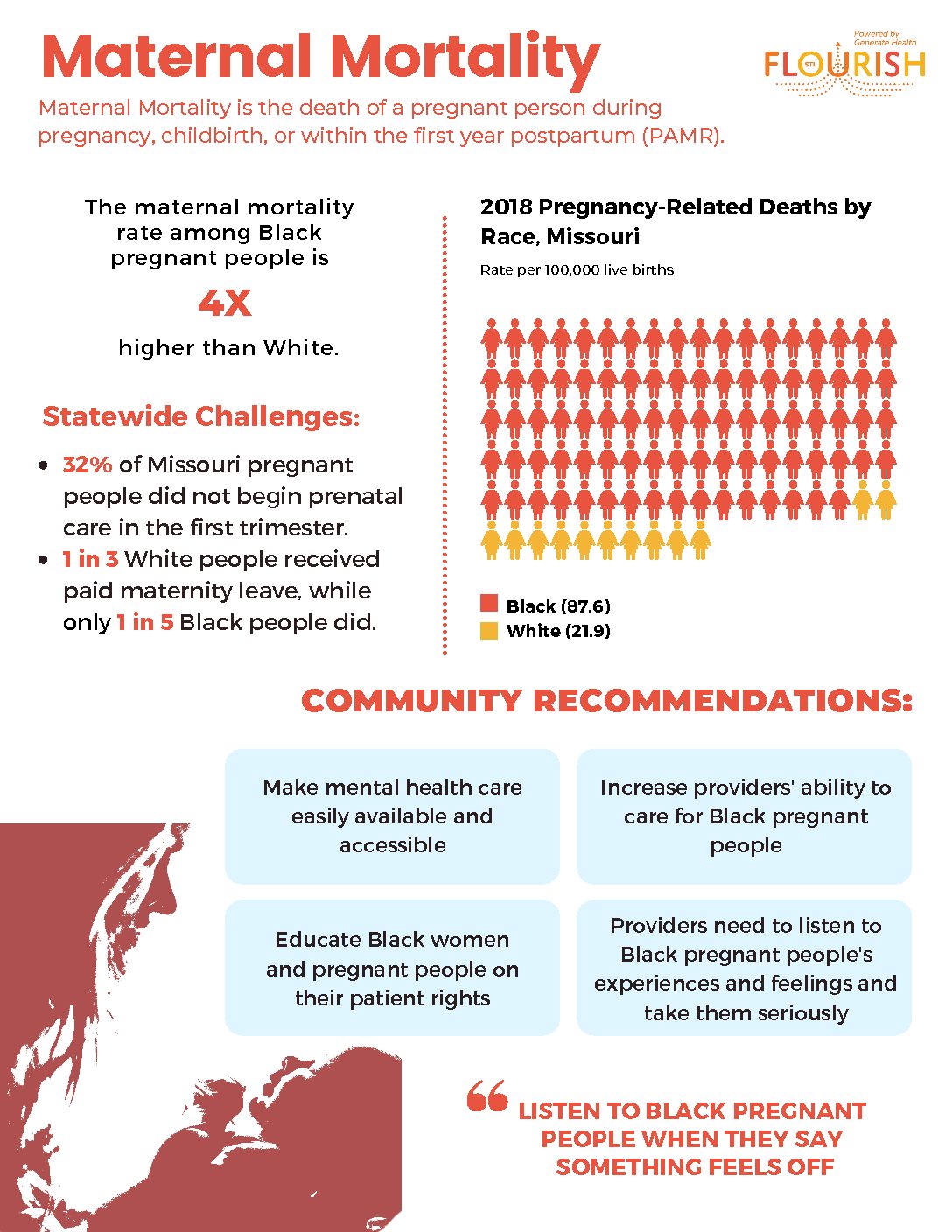
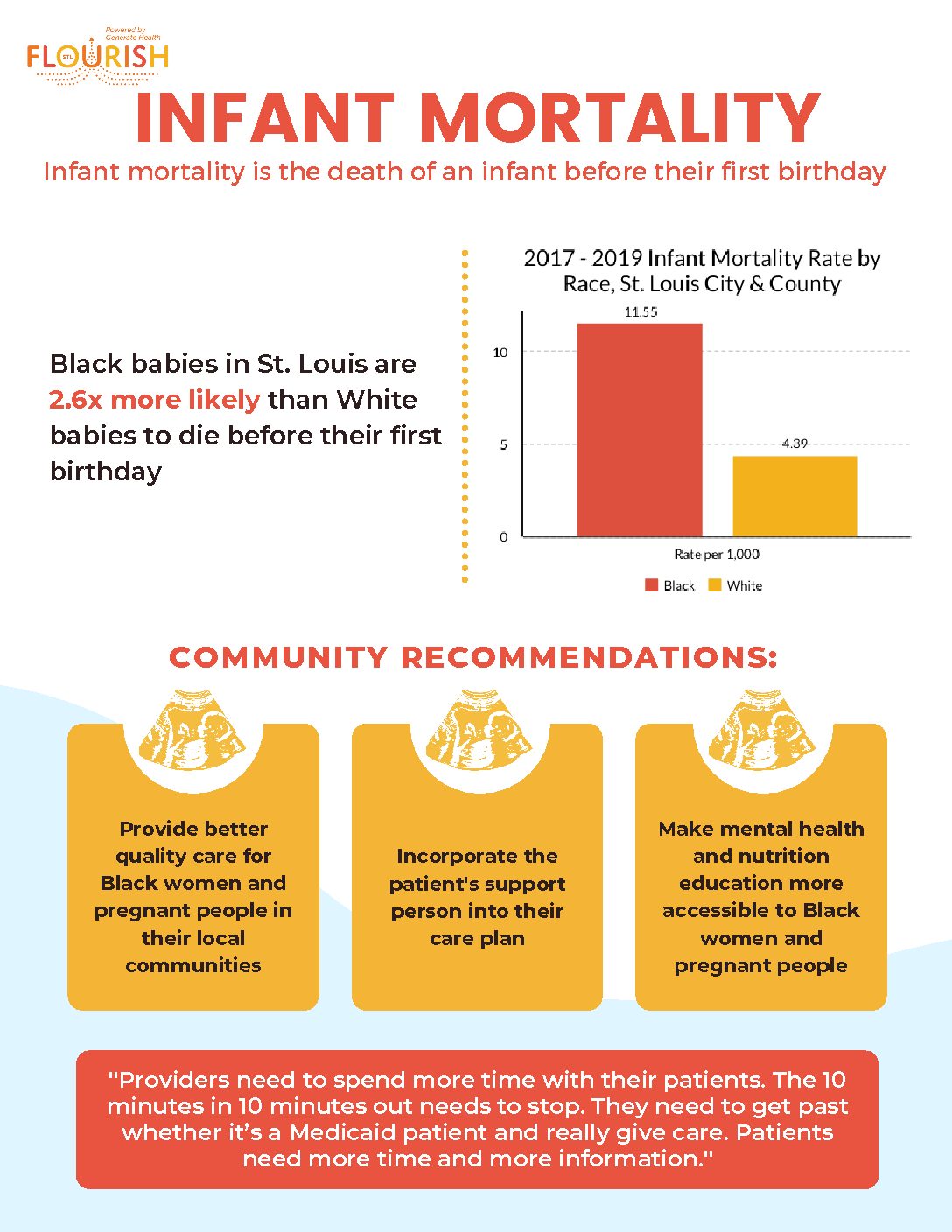
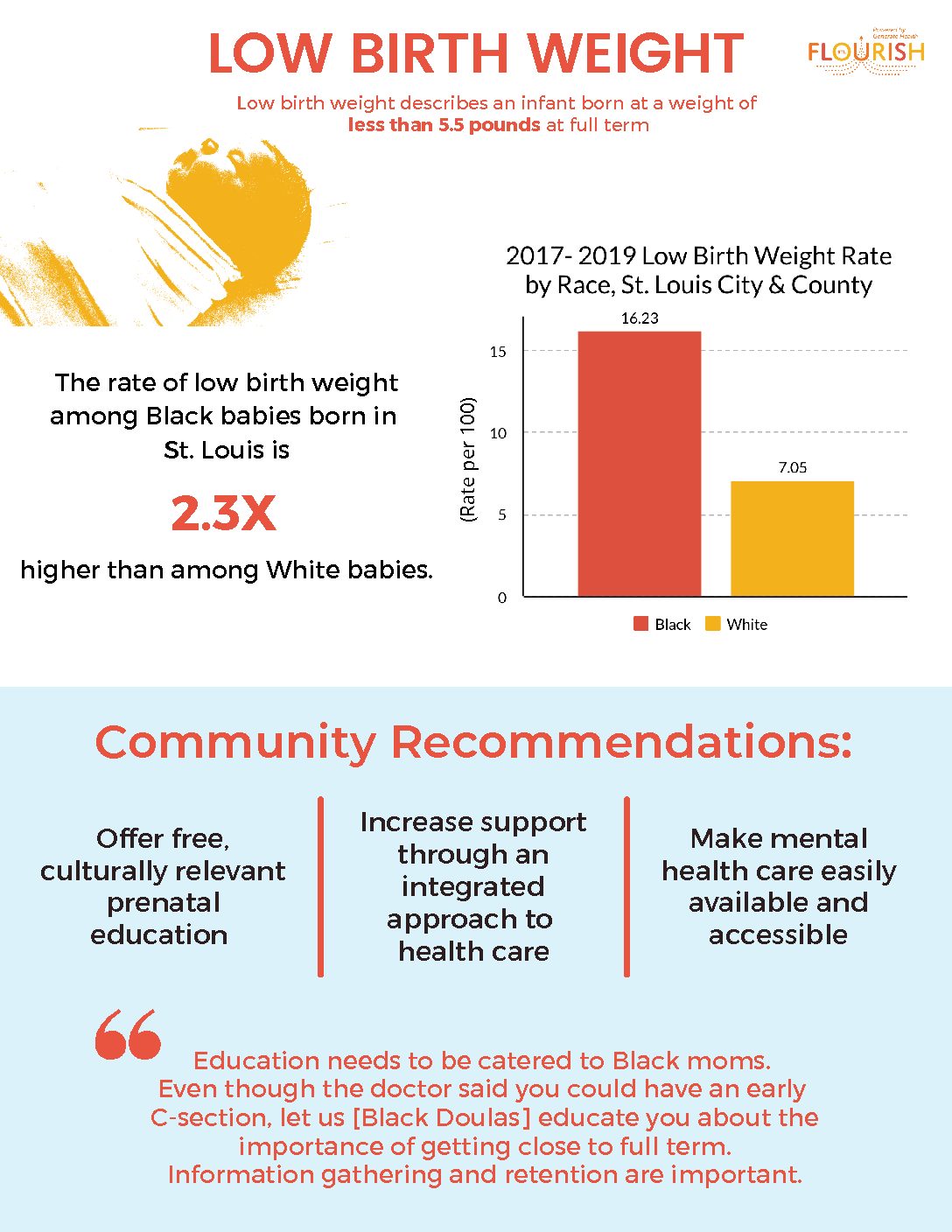
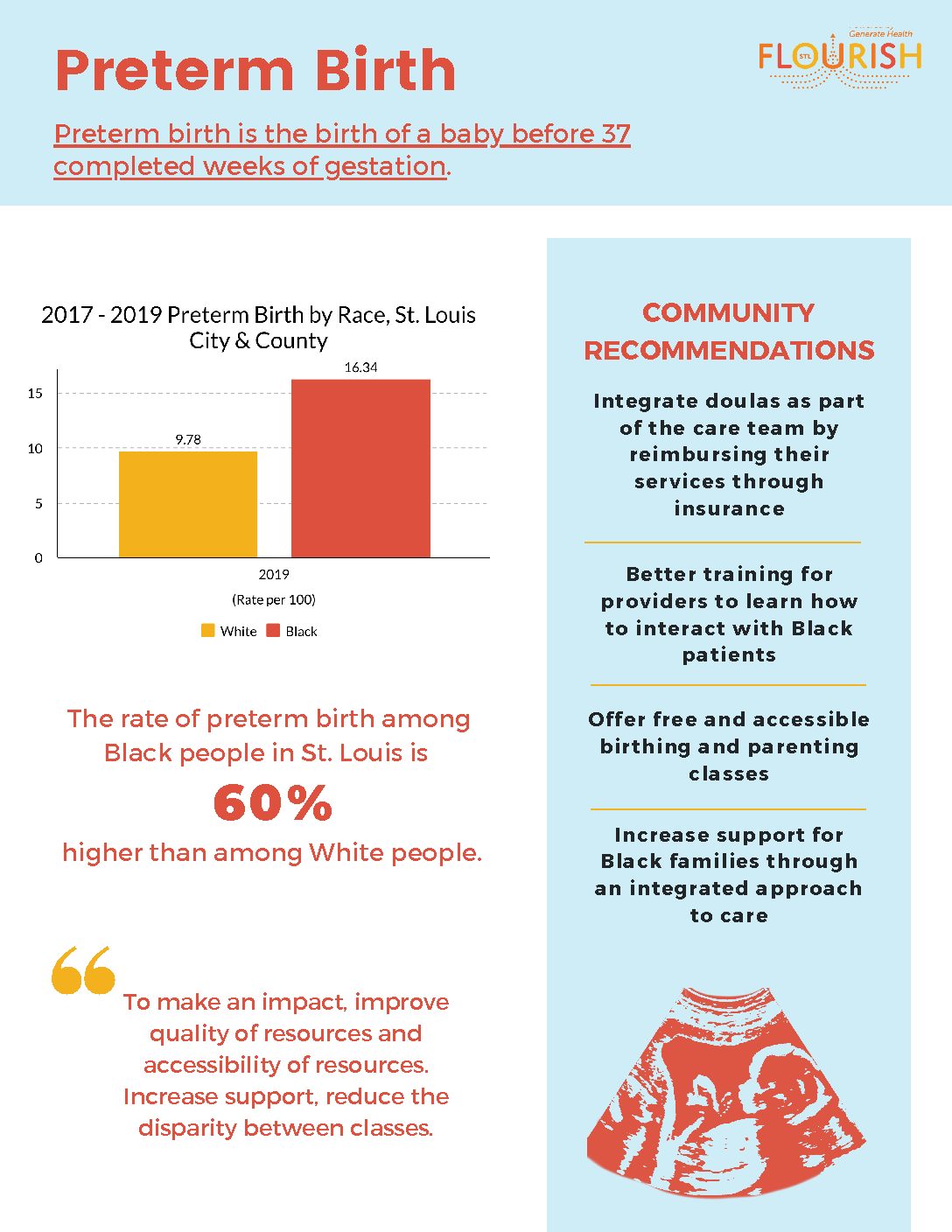
Despite being home to some of the best health care in the country, implicit bias among medical professionals plays a huge role in the health disparities in St. Louis. According to a 2019 Maternal and Child Health Profile, produced by the St. Louis County Department of Health, morbidity and mortality rates remain higher for Black families.